Using Brain Connectivity to Predict Treatment Response to Deep Brain Stimulation in OCD
Post by Thomas Brown
What's the science?
Deep brain stimulation (DBS) is a surgical procedure in which an electrode is placed into the brain of a patient, administering electrical pulses that regulate abnormal neuronal activity. DBS is most famous for its use in ameliorating tremors and dyskinesia in Parkinson’s Disease. Recent research has shown that DBS can also be effective in improving symptoms of psychiatric disorders including depression. Recent studies have also investigated the effectiveness of DBS in treating symptoms of obsessive compulsive disorder (OCD) in patients who don’t respond to treatment, however these studies have provided variable results. It is still unclear which patients respond well to DBS for OCD and what factors can predict good clinical outcomes. This week in Biological Psychiatry, Baldermann and colleagues assessed whether brain connectivity profiles can predict treatment outcomes after DBS in patients with OCD.
How did they do it?
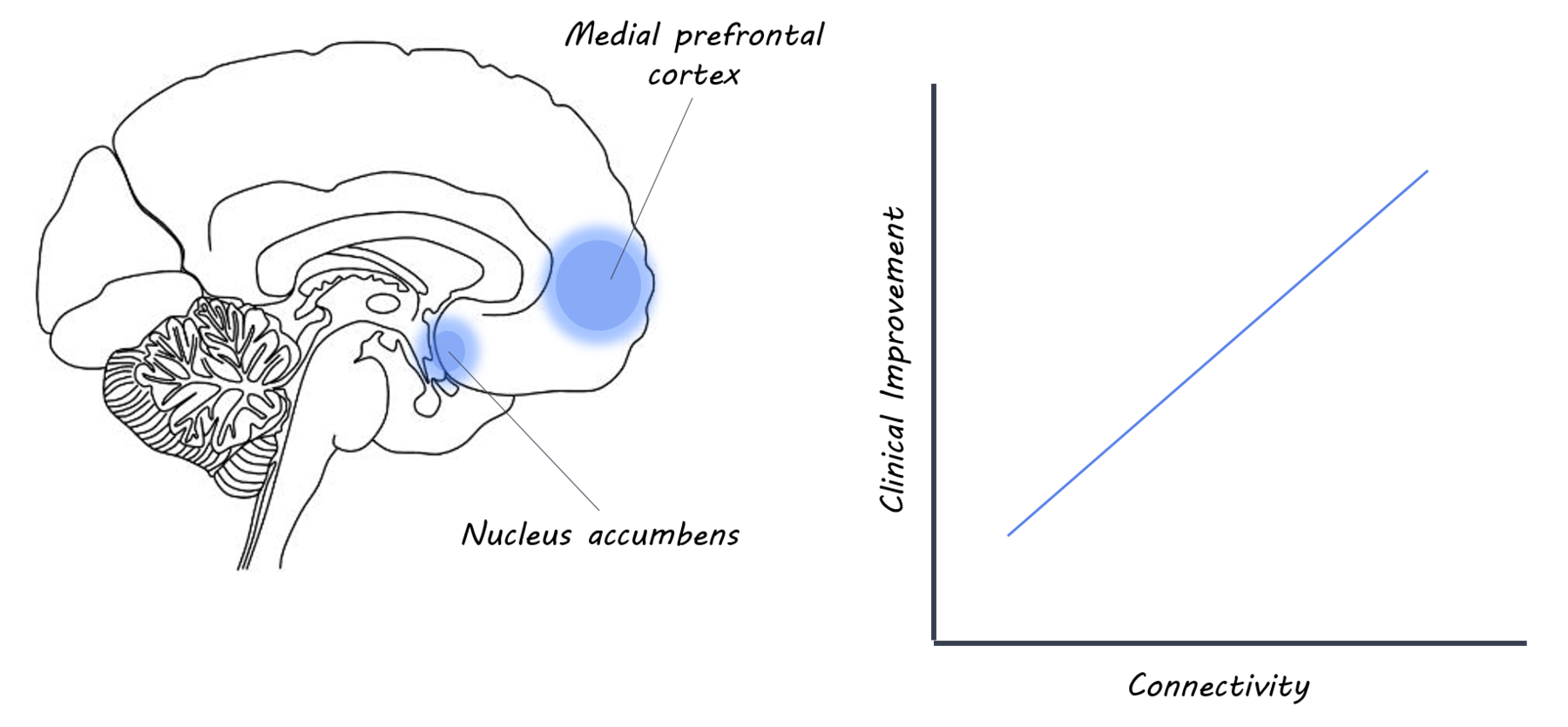
The authors recruited 22 patients with treatment-resistant obsessive compulsive disorder, who were undergoing DBS of the internal capsule/nucleus accumbens (an area of the brain which has been previously implicated in psychiatric conditions such as OCD). The authors acquired diffusion magnetic resonance imaging (dMRI) scans to measure the integrity of the brain’s white matter (connections) in a subgroup of 10 patients, in addition to an anatomical MRI scan (which looked at brain anatomy). Diffusion magnetic resonance imaging was used to visualise white matter tract connections within the brain. DTI is useful in understanding how a particular brain region is connected with the rest of the brain (i.e. a connectivity profile). The authors assessed connections between the internal capsule/nucleus accumbens and the rest of the brain (i.e. it’s connectivity profile). Brain imaging data from the Human Connectome Project was also used as a control group. Statistical tests were carried out in order to correlate connectivity patterns with a variety of factors, including clinical outcome one year post-surgery. The authors used connectivity maps specific to both patients and to healthy controls to test the relationships between connectivity and clinical factors in two separate subgroups of patients and then cross-validated using leave-one-out cross validation (in order to assess reproducibility). Finally, they combined the two subgroups for the main analysis.
What did they find?
In patients who had one year of DBS treatment and lower OCD severity, the authors found increased connectivity between the internal capsule/nucleus accumbens and the medial and lateral prefrontal cortex (bilaterally). They also found that increased connectivity between the stimulation site and the middle frontal gyrus was correlated with clinical improvement of OCD symptoms. This indicates that changes in connectivity can be used to predict whether DBS treatment had a positive clinical outcome.
What's the impact?
This study demonstrates a correlation between structural brain connectivity and severity of OCD. Secondly, it provides evidence that this connectivity can be used to predict clinical outcomes as well as identifies several brain targets to inform future OCD studies. These findings suggest that in combination with structural brain imaging, DBS could be a useful tool in treating patients with OCD. Finally, it demonstrates that electrical brain stimulation can change brain connectivity, providing further evidence for that DBS may exert its effects by modifying brain connectivity.
Baldermann et al., Connectivity profile predictive of effective deep brain stimulation in obsessive compulsive disorder. Biological Psychiatry (2018). Access the original scientific publication here.