An Optimal Amount of Sleep for Cognitive Function in Preclinical Alzheimer’s Disease
Post by Megan McCullough
The takeaway
There is an optimal amount of sleep that supports cognitive function in older individuals at risk of developing Alzheimer’s disease. Too little or too much sleep is correlated with a decrease in cognitive function over time.
What's the science?
Alzheimer’s disease is a neurological disorder characterized by cognitive decline and dementia. Pathologically, it is marked by an increase in the abnormal buildup of proteins, such as amyloid and tau in the brain. Previous studies have implicated sleep disturbances in the pathology of Alzheimer’s by relating abnormal sleeping patterns to cognitive decline. However, these studies have not considered the participants’ Alzheimer’s disease biomarkers or genetic risk factors for the disease. This week in Brain, Lucey and colleagues aimed to study the relationship between sleep and cognitive function while controlling for biomarkers associated with Alzheimer’s.
How did they do it?
The participants included 100 older adults who were at risk for developing Alzheimer’s. The authors measured the sleep-wake activity of the participants over the course of 4-6 nights. Sleep was measured using an EEG device worn on the forehead. The participants also underwent standardized cognitive assessments, genotyping for genes associated with the disease, and tests for the buildup of abnormal proteins. Statistical analyses were then conducted to study the relationship between sleep patterns and cognition over time, controlling for Alzheimer’s biomarkers.
What did they find?
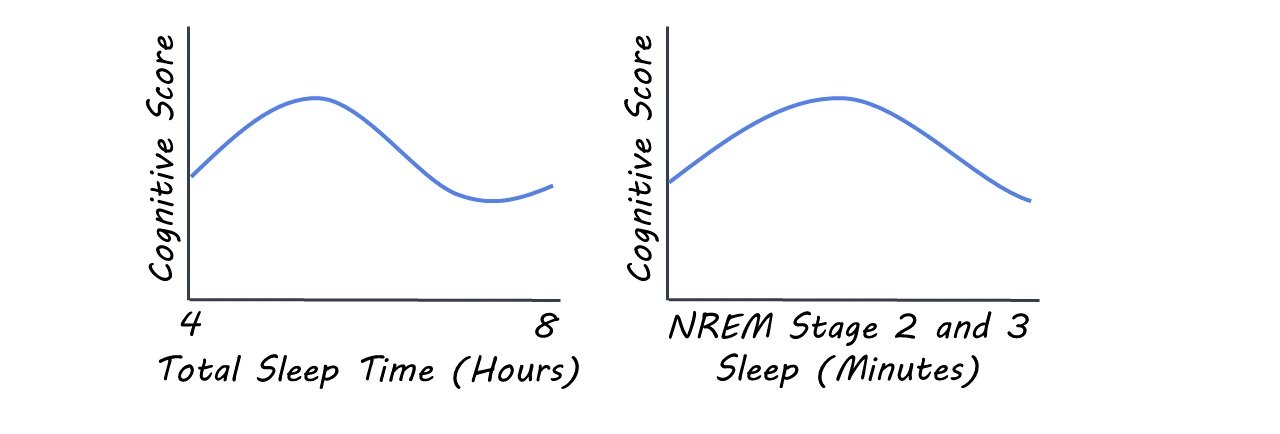
The authors found an inverse U-shaped relationship between sleep activity and cognitive performance over time. Cognitive scores were lower for individuals that slept less than about 4.5 hours or more than about 6.5 hours per night, with time asleep determined via EEG activity. The cognitive scores of individuals that slept between this range stayed stable. This relationship also held true when other measures of sleep activity were studied including time spent in REM and non-REM sleep phases. The same non-linear relationship was also seen when the data was adjusted for age and biomarkers of the disease. This suggests that there is an optimal range of time spent sleeping that supports cognitive function in individuals at risk of developing Alzheimer’s disease.
What's the impact?
This study is the first to show that an inverse U-shaped relationship exists between sleep activity and cognitive function even when participants were characterized by the presence of Alzheimer’s biomarkers. This is important as it suggests that there is a range of hours slept per night that supports cognitive function, even in individuals at risk for developing Alzheimer’s. These findings suggest that therapeutic efforts to optimize sleep duration could have a stabilizing effect on cognition.
Lucey et al. Sleep and longitudinal cognitive performance in preclinical and early symptomatic Alzheimer’s disease. Brain (2021). Access the original scientific publication here.