Pinpointing Target Regions for Brain Stimulation in Treatment-Resistant Depression
Post by Natalia Ladyka-Wojcik
The takeaway
This is the first large-scale randomized controlled trial to demonstrate the importance of pinpointing target regions involved in depression with magnetic resonance imaging (MRI) for treatment with transcranial magnetic stimulation (TMS). Treatment benefits can last longer than we previously understood - up to six months after TMS.
What's the science?
Although antidepressants and psychotherapies are effective treatment methods for many people with severe major depressive disorder, some individuals have treatment-resistant depression and may benefit from therapeutic neuromodulation, such as repetitive transcranial magnetic stimulation (rTMS). rTMS for depression has been popular for the past several decades, but – critically – no data is available to support its long-term effectiveness (beyond 1-3 months). Moreover, rTMS is traditionally applied to the same site on the scalp such that individual differences in the brain circuits involved in depression may not be accounted for. A more recent approach called connectivity-guided intermittent theta burst stimulation (cgiTBS), may provide longer-lasting treatment effects than standard rTMS by personalizing the targets to each individual’s brain circuitry using MRI data. This month in Nature Medicine, Morriss and colleagues directly compared the efficacy of both therapeutic neuromodulation approaches in a multi-center, randomized controlled trial for treatment-resistant depression over 26 weeks.
How did they do it?
Participants in this study were randomly assigned to receive 20 sessions of either rTMS or cgiTBS over four to six weeks. For both groups, sessions involved placing an electromagnetic coil against the scalp to deliver magnetic pulses that can alter activity in brain circuits thought to be involved in depression. The authors pinpointed the precise location of a brain region involved in depression (the left dorsolateral prefrontal cortex) for each participant by collecting structural or functional MRI (think brain anatomy vs. brain activity) for those undergoing rTMS or cgiTBS, respectively. cgiTBS coordinates were based on the correlation between brain activity of the left dorsolateral prefrontal cortex and the right anterior insula. Crucially, a computerized tracking system, called Neuronavigation, allowed them to deliver the treatment consistently across all 20 sessions, reducing the variability in stimulation at each session. To determine if participants showed a long-lasting reduction in depression symptoms following rTMS or cgiTBS, they administered a widely used depression assessment scale at the start of the study, and later at 8, 16, and 26 weeks.
What did they find?
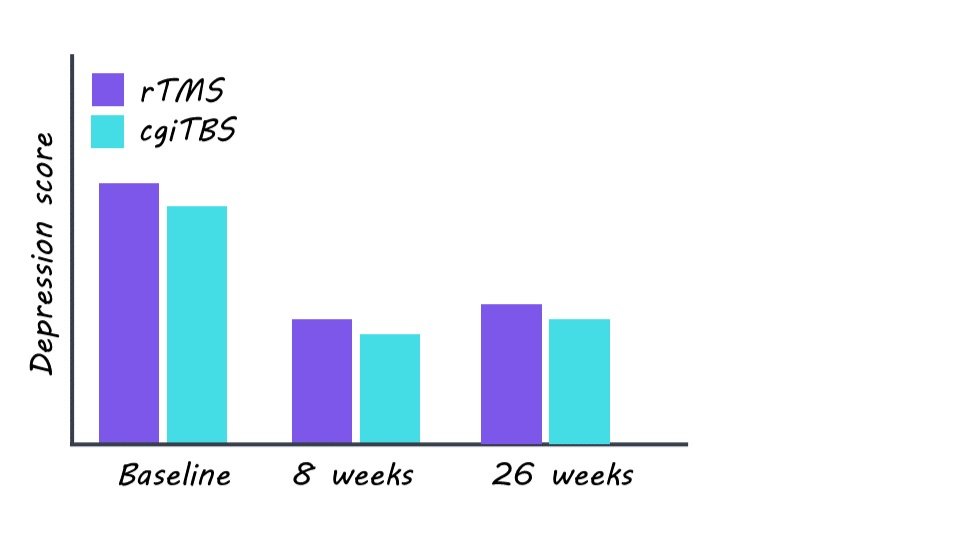
This study provides large-scale evidence for both rTMS and cgiTBS as effective interventions for treatment-resistant depression. Both groups showed a similar and large average decrease in symptom scores on the depression assessment scale at the 8-week follow-up compared to the start of the study and both groups maintained lower symptom scores on average at the 26-week follow-up. Participants experienced improvements in quality of life despite previously not responding to other treatment approaches for depression, with over two-thirds having reported feeling better by session 20 of stimulation. Importantly, a third of participants across both rTMS and cgiTBS groups showed a 50% drop in depression symptoms, with a fifth of participants maintaining this drop even after 26 weeks. The authors also found that participants who completed fewer than 20 stimulation sessions of either rTMS or cgiTBS showed less improvement in their depressive symptoms at the 26-week follow-up. Together, these findings demonstrate that personalizing the targeted brain sites (via either functional or structural means) for TMS using MRI in patients with treatment-resistant depression can result in long-lasting reductions of depression symptoms, even beyond what has previously been assessed in the literature.
What's the impact?
This study is the first large-scale trial to find evidence that MRI-guided TMS (both rTMS and cgiTBS) is an effective, long-lasting approach for treatment-resistant depression. Given that around a third of all people with major depressive disorder experience treatment-resistant depression which does not respond to antidepressants and psychotherapies, the results of this study highlight the need to establish MRI-guided TMS as a standard treatment approach in these cases.