Understanding Compulsive Disorders
Post by Laura Maile
What is compulsion?
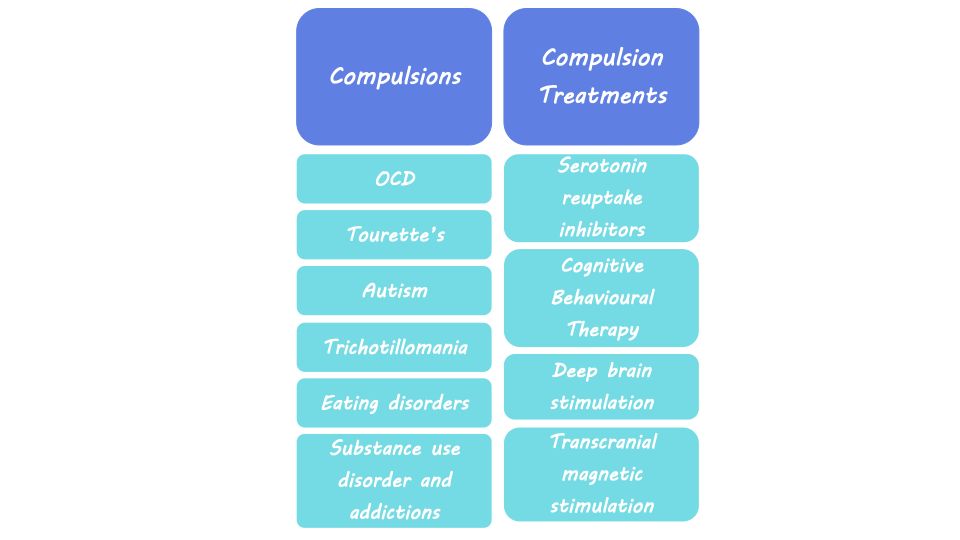
Compulsions are described as persistent urges to perform a specific behavior, even when the consequences are negative. They induce a feeling that the individual must complete the behavior, even though it may conflict with their overall goal. These repetitive behaviors are maladaptive, meaning they prevent individuals from adapting to their environment and are detrimental to overall well-being. Compulsions are a symptom of diseases like Obsessive Compulsive Disorder (OCD) and Tourette’s Syndrome, but they can occur in many other psychiatric disorders including Autism Spectrum Disorder, trichotillomania, eating disorders, substance use disorder, and other addictions. While compulsivity is a maladaptive symptom of disease, it can also be a component of everyday human behavior that leads to positive outcomes, including behaviors such as proofreading or athletic performance rituals.
Neurological basis of compulsive behavior
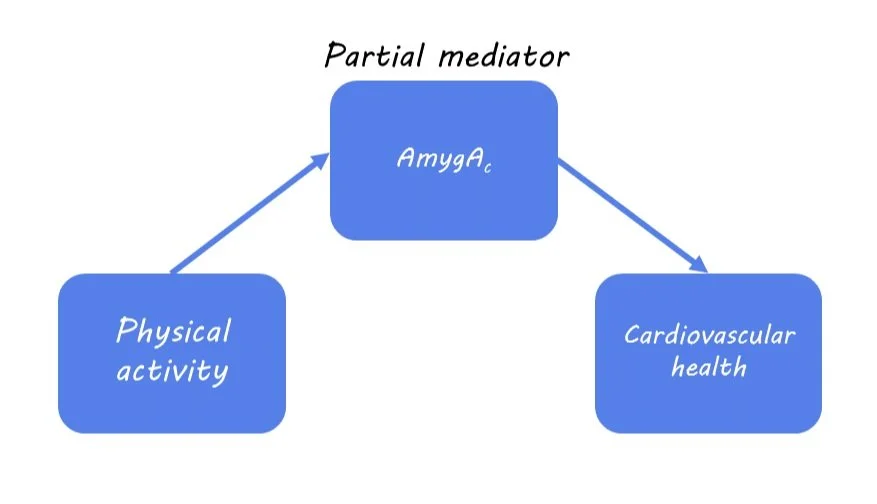
Some theories of compulsive behavior, which generally include ideas of positive and negative reinforcement learning, suggest that the neural networks that control goal-directed behavior and habits are out of balance. These networks include brain regions important for goal-directed and habitual behavior like the striatum, a part of the basal ganglia, which is important for controlling motor behavior, learning, and decision-making. In rodent studies where drugs are administered to inactivate specific areas of the striatum, habitual seeking of food and alcohol is reduced. Rodent studies also show that compulsive behavior can be born out of negative reinforcement, or avoidance of negative outcomes. The emergence of this compulsivity is dependent on brain systems required for habit formation like the striatum. The medial prefrontal cortex (mPFC) is also important for goal-directed behavior, habit formation, behavioral flexibility, the association between actions and outcomes, and decision-making. The nearby orbitofrontal cortex (OFC), a region involved in decision-making related to reward and emotion, is also likely involved in compulsive behavior. Another region implicated in goal-seeking and habitual behavior is the amygdala, which is part of the limbic system associated with emotion, fear, and aspects of learning and memory that are influenced by emotionally important stimuli.
Compulsive behavior can result when there is an imbalance or impairment in these networks that regulate goal-directed behavior. Neuroimaging studies in the human brain suggest that changes in these brain regions that regulate behavior are related to compulsion. For example, studies show reduced brain volume (i.e., grey matter) and elevated brain activity in the OFC in individuals with OCD. Changes in neural connectivity between the prefrontal cortex and striatum are also seen in patients with OCD.
Human imaging studies of individuals with OCD and substance use disorder found reduced functional connectivity (i.e., neural synchrony between brain regions) and activity of prefrontal cortex regions, which correlated with compulsive behavior. This loss of connectivity in the regions governing goal-directed behavior suggests a loss of control over habitual behavior and an inability to inhibit future actions, leading to compulsivity. Changes in activity related to compulsivity have also been seen in the insula, a region of the cortex associated with interoception, or awareness of bodily feelings. Interoceptive feelings and insula activity may trigger habits that have been developed through experiences involving negative reinforcement. The variety of findings in human imaging studies demonstrates the complexity of these neural networks that interact to influence compulsive behavior and highlight the need for more detailed research.
Treating compulsive behavior
Treatments for OCD and compulsive behaviors associated with other psychiatric disorders include serotonin reuptake inhibitors, cognitive behavioral therapy, and deep brain stimulation. Deep brain stimulation includes the implantation of electrodes into the brain to allow for electrical stimulation of specific areas. Clinical studies have shown that deep brain stimulation of the nucleus accumbens, a region associated with reward, was successful at reducing compulsivity symptoms in OCD patients who did not respond to other forms of treatment. A less invasive form of treatment is transcranial magnetic stimulation, which uses a magnetic coil outside the skull to influence the activity of certain brain areas. Transcranial magnetic stimulation of the mPFC has been shown to reduce OCD symptoms in some patients. Other studies using this technology to stimulate regions like the OFC, striatum, and basal ganglia show some promise for treating intractable OCD, though results are mixed. Transcranial magnetic stimulation has also been successfully deployed to target regions of the prefrontal cortex to reduce compulsive drug seeking in patients with substance use disorder.
What's next?
While some success has been achieved with transcranial and deep brain stimulation, more research is needed to improve outcomes and reduce side effects of compulsive behavior. New deep brain stimulation techniques are being investigated that can deliver neurostimulation while recording neural activity, which will allow scientists more insight into the neural basis of compulsive behavior. Other novel treatments being studied for compulsive behavior include ketamine and psychedelics, which can be used as treatments for depression or anxiety. There is also ongoing work aimed at uncovering how findings related to the contribution of serotonin, dopamine, and noradrenaline to compulsive behavior translate from rodent to human systems.