Neuron to Neuron Information Transfer is Critical for Emotion Recognition and Social Cognition
Post by Soumilee Chaudhuri
The takeaway
Information transfer from the medial prefrontal cortex (mPFC) to the retrosplenial cortex (RSC) of the brain is crucial for emotion recognition - the ability to recognize and respond to the emotional states of others. This study found that inhibiting the mPFC-to-RSC brain pathway in mice affects their ability to recognize emotional states like stress and relief in their peers, shedding light on the neural mechanisms behind social cognition.
What's the science?
Emotion recognition is essential for appropriate social interactions, enabling individuals to respond to the emotional states of others. Recent research has revealed that recognizing emotions in others involves complex communication between different parts of the brain, but understanding the exact brain pathways involved has been challenging. This study in Nature Neuroscience by Dautan et. al., delves into the mPFC-to-RSC pathway, focusing specifically on the role of somatostatin (SOM) neurons that project from the mPFC to the RSC. SOM neurons are known for their inhibitory role in the brain - they produce Gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter. It is also known that these SOM neurons help filter and process socially derived information, enabling accurate emotion recognition. In this study, researchers used optogenetics to manipulate the mPFC-to-RSC SOM neurons and observe their impact on the behavior of the mice.
How did they do it?
In this study, researchers utilized a combination of behavioral tests, optogenetics, and calcium imaging to investigate how information transfer between the mPFC and RSC affects emotion recognition in mice. The focus was on the interaction between specific neuron types, including pyramidal neurons in the RSC and SOM neurons in the mPFC. They specifically targeted genetically modified SOM neurons that expressed light-sensitive proteins. Light was used to either activate or inhibit these neurons and behavioral tests in mice assessed their emotions during these periods of activation or inhibition. Behavioral tests in mice included a series of assessments wherein mice had to recognize emotional states (stress or relief) in other mice. By stimulating or inhibiting the SOM neurons in the mPFC, researchers could observe changes in the mice's ability to recognize these emotional cues and record their responses.
What did they find?
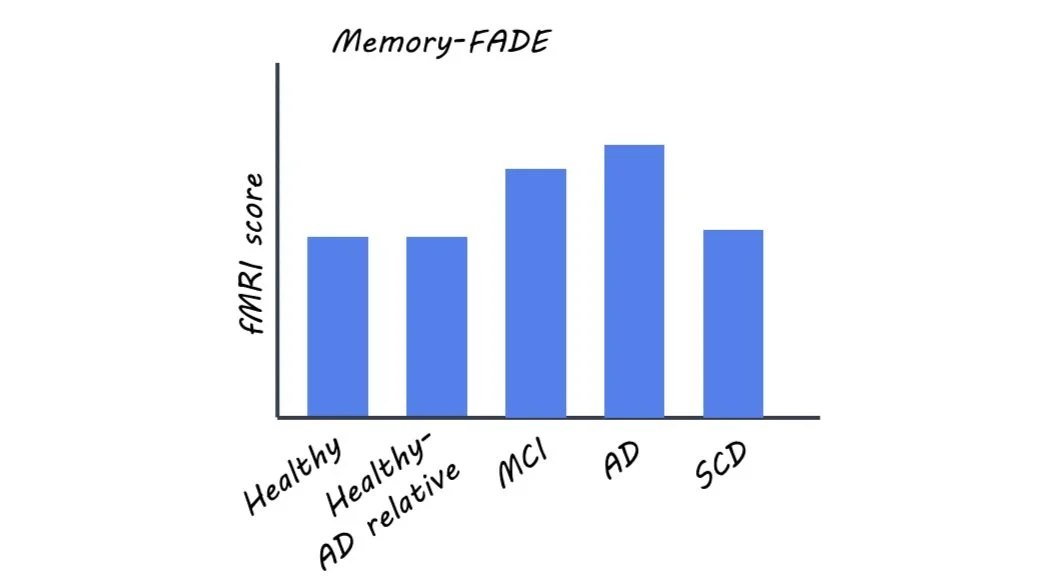
The researchers found that inhibiting the mPFC-to-RSC pathway impaired the mice's ability to recognize emotions in their peers while stimulating it enhanced their emotional recognition capabilities. The results indicated that SOM neurons in the mPFC regulate the activity of RSC pyramidal neurons, influencing how mice process and respond to social and emotional stimuli. When the mPFC-to-RSC SOM neurons were inhibited, the activity of RSC pyramidal neurons increased, indicating that the SOM neurons help regulate the signal-to-noise ratio within the RSC. This regulation of mPFC SOM neurons to RSC pyramidal neurons was vital for processing and interpreting social and emotional stimuli accurately and it was shown that about 10% of mPFC SOM neurons project to RSC and thus modulate the activity of RSC pyramidal neurons. Interestingly, these results in mice were similar to what other scientists have observed in recent functional magnetic resonance imaging(fMRI) studies in humans.
What's the impact?
Understanding the mPFC-to-RSC pathway's role in emotion recognition has significant implications for studying social cognitive disorders like autism and schizophrenia, where emotion recognition is often impaired. This research offers avenues for therapeutic strategies targeting specific brain pathways to improve social functioning. Additionally, it provides a deeper understanding of the neural mechanisms underlying social behavior and emotional processing, which could inform future studies in both animals and humans.