Stimulating an Entorhinal Cortex Circuit is Antidepressive
What's the science?
Major depressive disorder can lead to many structural and functional changes in the hippocampus, including slowed neurogenesis (new neuron formation). Stimulation of the entorhinal cortex (which sends information to the hippocampus) can improve learning and memory. It is possible that entorhinal cortex stimulation could also relieve depression. Current depression therapies, including transcranial magnetic stimulation and electroconvulsive therapy, often have side effects, so more treatment options are needed. This week in Nature Medicine, Yun and colleagues test whether stimulating an entorhinal circuit is antidepressive in mice and uncover the mechanisms involved.
How did they do it?
They knocked down a protein subunit (TRIP8b) of a protein channel (hyperpolarization channel) using a viral-mediated approach which reduces the number and sensitivity of these protein channels found on neurons. This increases the excitability of neurons in the entorhinal cortex. The hypothesis was that increased excitation in the entorhinal cortex would increase neurogenesis in the hippocampus, and in turn reduce depressive behavior in mice. They performed several experiments: They tested whether psychosocial stress (a model of depression) increases TRIP8b levels in neurons. Using viral-mediated TRIP8b knockdown, they confirmed the increased excitability of entorhinal cortex neurons that project to the hippocampus (dentate gyrus). They measured neurogenesis in the hippocampus (dentate gyrus) in TRIP8b knockdown and controls. They then tested whether antidepressive behavior and memory were changed in knockdown vs. controls and whether this was dependent on neurogenesis. Lastly, they used gene transfer and transgenic mice combined with chemogenetics to activate glutamatergic neurons (i.e. excitatory neurons) in the entorhinal cortex, in order to observe the effects on antidepressive behavior.
What did they find?
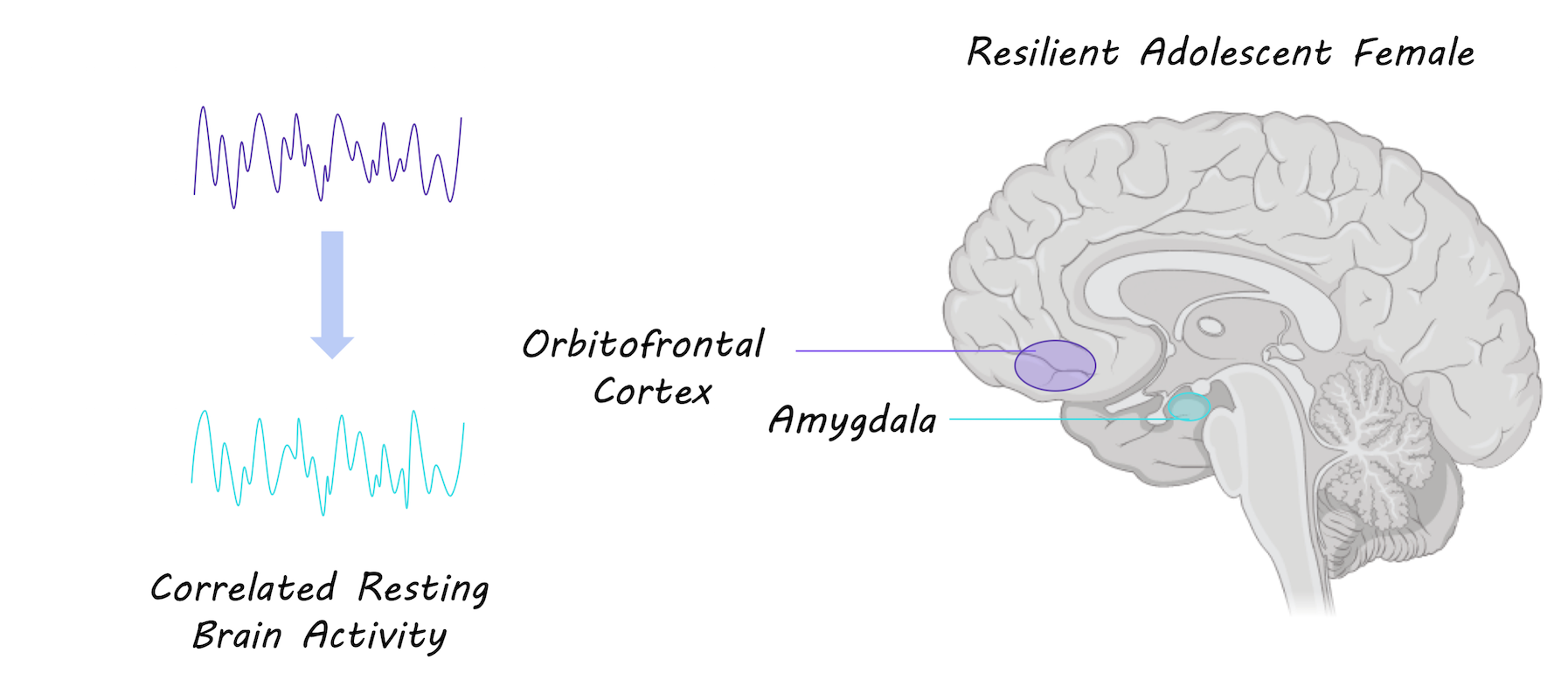
They found that psychosocial stress in mice resulted in increased levels of TRIB8b in entorhinal neurons that project to the dentate gyrus. After knockdown of TRIP8b, they found increased excitability of entorhinal cells and increased neurogenesis in the connected hippocampus (in the dentate gyrus), confirming the hypothesis that increased activity in the entorhinal cortex results in neurogenesis in the hippocampus. TRIP8b knockdown in the entorhinal cortex also resulted in antidepressive-like behavior and improved memory in mice. To test whether this was dependent on neurogenesis in the hippocampus, they used X-ray irradiation to ablate new neurons and found that antidepressive behavior was dependent on hippocampal neurogenesis. Using chemogenetics to chronically stimulate glutamatergic neurons in the entorhinal cortex, they found that glutamatergic neurons drove neurogenesis in the hippocampus and were responsible for antidepressive behavior.
What's the impact?
This is the first study to show that activity in the entorhinal-hippocampal circuit results in both the formation of new neurons in the hippocampus and antidepressive behaviors in mice. Altering activity in this entorhinal cortex circuit - previously appreciated only as a memory circuit - by stimulating it could be a new way to reduce symptoms of depression in humans.
S. Yun et al., Stimulation of entorhinal cortex–dentate gyrus circuitry is antidepressive. Nature Medicine (2018). Access the original scientific publication here.