Connectivity of the Amygdala Predicts Risk Tolerance
What's the science?
Risk can be thought of as uncertainty — when there is some information about the possible outcome of a situation. Different individuals have different tolerance for risk when making decisions. We know that certain brain regions are generally involved in risk perception from studies looking at brain activation during risk (e.g. medial prefrontal cortex, anterior insula, anterior cingulate cortex, amygdala), however, we don’t know which brain regions and which inherent properties of these brain regions affect individual risk tolerance. This week in Neuron, Jung and colleagues use a data-driven approach to determine which brain regions and functional properties of these regions predict individual risk tolerance.
How did they do it?
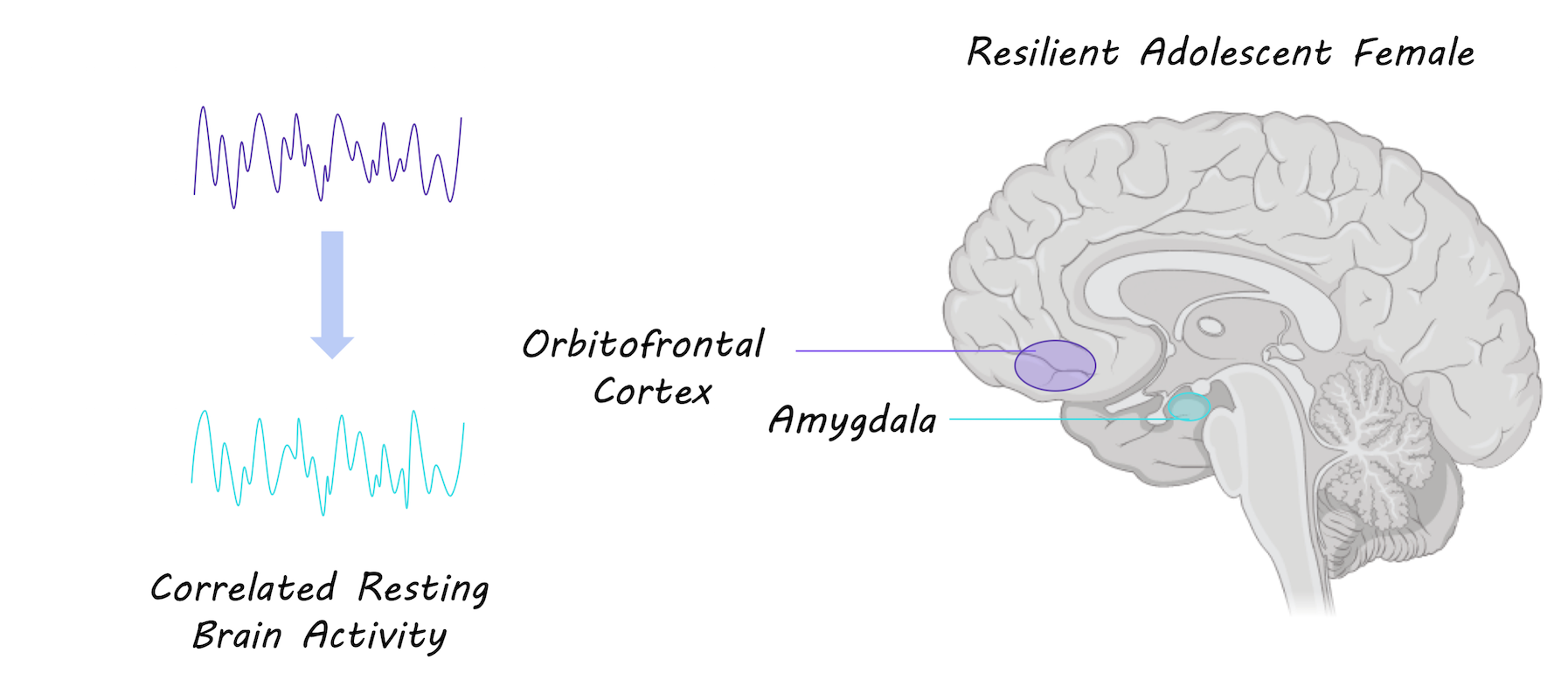
Anatomical MRI, resting-state MRI (brain activity at rest) and Diffusion Tensor Imaging (structural connectivity) data from 108 healthy adults were acquired. Participants also performed a well-validated risk task to assess their risk tolerance. This task involves making binary decisions over several trials, choosing between a certain monetary reward and a larger uncertain (i.e. riskier) reward. They first analyzed the resting-state MRI data to compute individual functional connectivity throughout the brain (synchrony between brain regions at rest) to determine important regions that show a large amount of synchrony with other brain regions (i.e. highly central brain regions). In an exploratory, data-driven approach, they then assessed whether the strength of the functional connectivity in any these regions throughout the brain predicted individual risk tolerance.
What did they find?
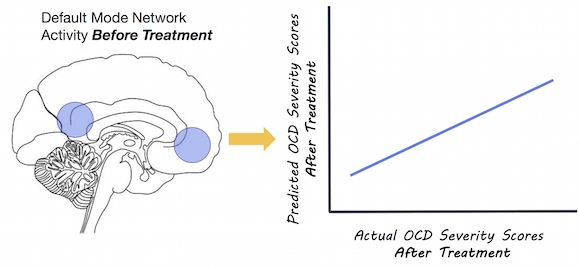
The strength of functional connectivity in the amygdala showed the strongest correlation with risk tolerance of any brain region. Based on this finding, the authors focused on the amygdala for the remainder of their analyses. They tested which specific functional connections of the amygdala were important for risk tolerance. They used the amygdala as a seed region and found that the medial prefrontal cortex showed the strongest functional connections. There was a positive correlation between risk tolerance and functional connectivity between the amygdala and the medial prefrontal cortex; greater risk tolerance was associated with stronger functional connections. They then assessed whether the structural connectivity (white matter tracts) between the amygdala and the medial prefrontal cortex was associated with risk tolerance, and found that there was a negative correlation between structural connectivity and risk tolerance; stronger white matter tract connectivity was associated with lower risk tolerance (significant for the right amygdala, and trending for the left amygdala). They also found that more gray matter volume in the amygdala was associated with a higher risk tolerance. In a regression analysis, they found that functional connectivity, gray matter volume and tract strength (only on the right) were all predictors of individual risk tolerance.
What's the impact?
This is the first study to show that the inherent properties of the amygdala and its’ connections are associated with individual risk tolerance. This study suggests that an individual’s brain structure and function, which can be thought of as their “brain signature” can be used to predict individual behavior. Localizing brain regions involved in risk tolerance is important for understanding why some individuals engage in risk-taking behavior.
W.H. Jung et al., Amygdala Functional and Structural Connectivity Predicts Individual Risk Tolerance. Neuron (2018). Access the original scientific publication here.